Understanding Motor Impairments in Autism: What Parents Need to Know
When we think about autism, we often focus on social communication, behavior, or language challenges. But there’s another major piece of the puzzle that often gets overlooked: motor planning challenges.
If your child with autism struggles with movement—whether it’s balance, coordination, or learning new motor tasks—you are not alone. And most importantly, it’s not just clumsiness. Research now shows that the motor challenges many children with autism face may actually represent a distinct motor disability—one that doesn’t fit neatly into current diagnostic boxes like “fine and gross motor skill delays.”
Let’s break down what this means, why it matters, and how you can support your child.
A Different Kind of Motor Difficulty
Motor difficulties are incredibly common in children with autism—affecting up to 80% of them. But these aren’t just the same as the challenges seen in other movement disorders. Emerging research shows that the motor profile in autism is qualitatively different—meaning it doesn’t just look different on the surface, it functions differently at a neurological level.
Children with autism often struggle with motor planning, gesture imitation, timing, and coordination of complex movements. This can affect everything from walking and jumping to using a spoon, getting dressed, or learning to write. While some of these struggles may overlap with apraxia or DCD, they show up in a uniquely different way for autistic children.
Researchers like Kilroy and colleagues (2022) have shown that while children with autism may have similar fine and gross motor delays as those with DCD, they tend to have more difficulty with gesture imitation, movement on demand, and spontaneous actions. These types of movements require the brain to plan, organize, and execute coordinated sequences—something that appears to be especially disrupted in autism.
Why Is Movement So Hard for Some Kids With Autism?
At the core of these motor challenges is something called neuromotor dysfunction. In simple terms, the brain is having trouble sending accurate, timely signals to the body to perform a specific movement.
Studies using brain imaging and motion tracking (like those by Vasa et al., 2016 and Emanuele et al., 2021) have found that children with autism often show:
- Increased movement variability (i.e., inconsistent and unpredictable movements)
- Less efficient coordination between joints and muscles (called motor synergies)
- A tendency to rely less on visual feedback when moving
- Difficulties with sensorimotor integration—how the brain interprets sensory input and transforms it into motor output
This can result in movement that looks hesitant, fragmented, or repetitive—not because a child doesn’t understand what to do, but because their motor system can’t organize the action effectively.
It’s Not Just About Speech or Coordination
While some children with autism are diagnosed with Childhood Apraxia of Speech (CAS) or Developmental Coordination Disorder (DCD), these labels often fall short in capturing the full scope of motor issues they experience.
For example:
- A child may be able to talk, but still struggle with initiating movement like waving, brushing teeth, or copying a simple action.
- A child may score low on coordination tests, but their real struggle lies in their brain’s ability to plan and carry out whole-body movements, not just isolated actions.
In fact, Minissi et al. (2023) found that when autistic children engaged in natural, full-body tasks like kicking a ball or blowing bubbles, they needed more time to plan and execute movements, and their movements were often awkward or disjointed. This points to deeper issues with praxis—the brain’s ability to turn a motor intention into coordinated action.
So… Is It Apraxia? Is It DCD? Or Something Else?
That’s the big question. And unfortunately, right now, the answer isn’t simple.
Despite decades of research showing significant motor challenges in autism, most children are not being formally diagnosed with any motor disorder. A recent review (Kangarani-Farahani et al., 2024) showed that only 3 out of 27 studies on motor impairment in autism used a DCD diagnosis, even though up to 88% of children showed clear motor delays.
Why the disconnect?
Because the motor issues in autism don’t fully match existing categories like apraxia or DCD. They’re more widespread, more variable, and more rooted in neurological differences than in isolated skill deficits. Many children with profound autism are falling through the cracks of a system that wasn’t built to recognize or respond to their unique motor profiles.
What This Means for You as a Parent
What research tells us is that these Motor Planning Challenges in Autism are real, biological, and often misunderstood. And that misunderstanding is affecting everything from how we diagnose to how we intervene.
Right now, therapists and professionals may focus on “surface-level” goals like:
- Tying shoes
- Holding a pencil
- Balancing on one foot
…without ever addressing the underlying problem—how the brain and body work together to create movement.
This is why many traditional therapies fall short. Without a deep understanding of motor planning, praxis, and sensory-motor integration, the interventions don’t go deep enough to make real change.
The Missing Link: A Neuromotor Framework for Autism
Researchers like Bhat (2022) and Torres et al. (2018) are now calling for a new way to understand motor impairments in autism—one that moves beyond checklists and embraces the complexity of how the autistic brain processes movement.
One promising model is based on sensory reafference and micromovements—subtle internal feedback loops the body uses to adjust and refine motion. In children with autism, these feedback systems appear to be disrupted, leading to movement that’s less precise, more variable, and harder to control. And that can impact everything from tying a shoe to participating in social play.
Until we build this new framework into everyday clinical practice, children with autism will continue to be underserved by therapies that don’t match their real needs.
So What Can You Do?
As a parent, you don’t need to wait for the system to catch up. Here’s how you can start advocating for better support today:
1. Ask for a Motor Evaluation
Request that your child be assessed not just for speech or behavior—but for whole-body motor skills. Look for occupational therapists or physical therapists familiar with autism, whole body apraxia, and neuromotor development.
2. Look Beyond the Labels
Don’t get stuck on whether your child “qualifies” for a specific diagnosis like DCD or apraxia. The goal is to understand how your child moves and where the breakdowns happen—so you can target the right kind of support.
3. Focus on Movement That Matters
Instead of isolated skill drills, prioritize activities that support motor planning, body awareness, and coordination across systems. Things like:
- Functional movement patterns (crawling, climbing, jumping)
- Imitation games
- Rhythm-based tasks
- Vision-motor exercises
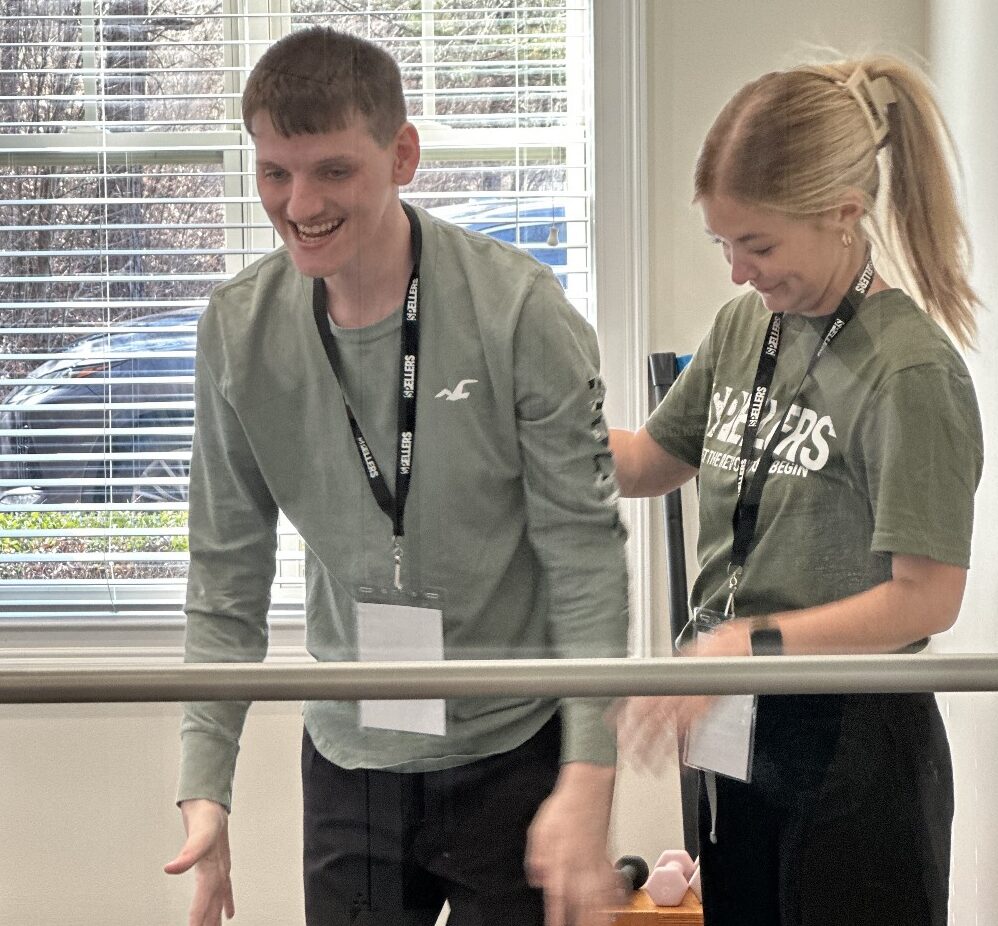
These are just some of the focal points in the therapy that we provide at Spellers Center Tampa.
4. Advocate for a Whole-Child Approach
Movement isn’t separate from communication, social skills, or learning. In fact, they’re deeply connected. A child who can’t control their body will struggle to participate, connect, and express themselves. Make sure your child’s team is addressing motor health as part of the whole picture.
Final Thoughts
Motor Planning Challenges in Autism, specifically, your child’s motor struggles are not your fault—and they’re not your child’s fault either. They’re part of a deeper, biological reality that many professionals are just beginning to understand.
But knowledge is power.
And as a parent, you can use this knowledge to ask better questions, demand better answers, and build a team that supports your child’s entire development—not just what’s easy to see.
Autism is not just about behavior. It’s also about movement. And when we address the motor system, we open the door to better communication, better regulation, and better outcomes.
Your child deserves nothing less.
Be sure to check out the Spellers Documentary to see how Spellers Method has impacted people lives.